🤝 Partner Spotlight
Find therapy that works - 25% OFF your first month
Anxious? Depressed?
Find Therapy that finally works for you. BetterHelp offers personal, reliable mental health support from the comfort of your home, with 25% off your first month of therapy.
72% of clients see reduced symptoms within 12 weeks. BetterHelp is also HSA + FSA eligible, with a network of 30,000 licensed therapist to support your needs. Why wait? Get matched in as little as 48 hours.
This email was delivered by a third-party, on behalf of BetterHelp. Copyright © 2025 BetterHelp. All Rights Reserved.
Issue #24: December 22, 2025
🩸 Beyond LDL: The Markers That Actually Tell the Atherosclerosis Story
If cholesterol were a courtroom case, LDL would be the prime suspect.
For decades, the story sounded simple:
High LDL clogs arteries.
Clogged arteries cause heart attacks.
Lower LDL, problem solved.
It was clean. Easy to explain. Easy to measure.
But also incomplete.
Modern lipid science has made something clear: atherosclerosis isn’t driven by cholesterol alone — it’s driven by particles, genetics, and the metabolic environment they move through.
That’s why two people with the same LDL can have very different cardiovascular risk. And why so many heart attacks still occur in people with “normal cholesterol.”
Before we go further, one important clarification: this isn’t an anti-statin piece. Statins lower both LDL-C and ApoB, and they work. The point here isn’t to reject treatment — it’s to understand whether a given LDL target is actually protective, or simply hitting an arbitrary lab value. That distinction matters.
🧪 LDL-C: What It Tells You (and What It Misses)
LDL-C measures the amount of cholesterol inside LDL particles.
What it doesn’t tell you:
How many LDL particles you have
Whether they’re large and buoyant or small and dense
How likely they are to penetrate and get trapped in artery walls
Two people can both have an LDL of 120:
One may have a few large particles
The other may have many small ones
Same cholesterol number. Very different biology.
LDL-C is like measuring how much luggage is in an airport — not how many planes are actually taking off and landing.
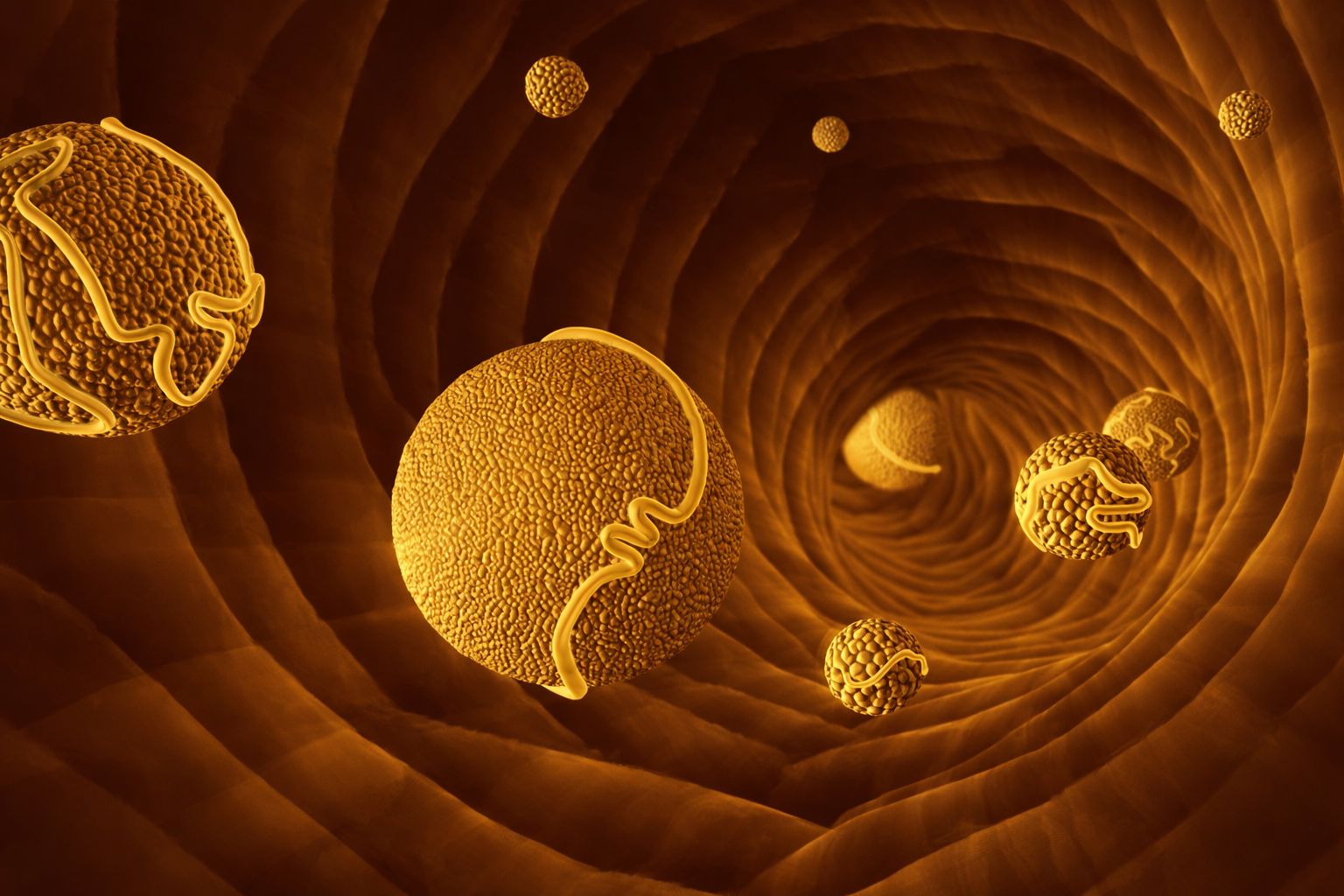
Atherosclerosis begins with particle entry, not cholesterol weight. And LDL-C can’t see that.
🔢 ApoB: Counting the Planes, Not the Luggage
This is where ApoB changes everything.
Every atherogenic particle — LDL, VLDL, IDL, remnants, and Lp(a) — carries exactly one ApoB100 molecule.
Which means:
ApoB reflects the total number of potentially harmful particles in circulation.
Not how much cholesterol they carry — but how many chances there are for one to get stuck.
This matters because plaque formation is probabilistic. More particles mean more opportunities for arterial retention.
That’s why ApoB consistently outperforms LDL-C as a predictor of cardiovascular events and mortality. People with “normal LDL” but elevated ApoB still carry meaningful risk.
📊 What Are Reasonable ApoB Reference Ranges?
<80 mg/dL: generally considered low risk
80–100 mg/dL: moderate risk (context matters)
>100 mg/dL: elevated risk (intervention often warranted)
Some longevity-focused protocols aim for <70 mg/dL, or even <60 mg/dL, especially in people with additional risk factors.
The key nuance: an ApoB of 95 in someone with low inflammation, excellent insulin sensitivity, and no Lp(a) is very different from the same number in someone with insulin resistance and chronic inflammation.
ApoB shows what’s happening under the hood — not just what’s floating in the bloodstream.
🧬 Lp(a): The Genetic Modifier Most People Never Measure
Lp(a) is a special LDL-like particle with an added protein — apolipoprotein(a) — attached to ApoB.
That extra protein makes it:
Stickier
More inflammatory
More likely to deposit in arteries
Capable of interfering with clot breakdown
High Lp(a) is largely genetic and affects roughly 20–30% of people worldwide.
The problem?
Standard lipid panels don’t measure it.
So many people are told their cholesterol is “perfect” without realizing they may be carrying a silent genetic risk amplifier.
Personally, this is one area where I got lucky:
Lp(a): <10
At this level, Lp(a) is not a meaningful contributor to cardiovascular risk.
Importantly, while diet and lifestyle don’t meaningfully lower Lp(a), some medications (PCSK9 inhibitors) reduce it by ~20–30%, and newer therapies targeting apolipoprotein(a) are currently in clinical trials. For very high Lp(a), this is a conversation worth having with a lipid specialist.
🔁 HDL & Triglycerides: Context is Everything
HDL is often labeled “good cholesterol,” but that label oversimplifies things.
HDL is protective when it’s functional — when it can remove cholesterol from arterial walls and exert anti-inflammatory effects. That function depends heavily on metabolic health.
This is where triglycerides become especially useful.
Elevated triglycerides often reflect:
Excess glucose flux
Insulin resistance
Overproduction of lipoproteins
A shift toward small, dense LDL particles
Low triglycerides usually suggest the opposite
In my own labs:
HDL: 94
Triglycerides: 48
That low TG-to-HDL ratio signals efficient fuel use, good insulin sensitivity, and a lipid system under relatively low stress.
Single numbers rarely tell the story. Patterns do.
🔥 The Metabolic Terrain: Where Risk is Actually Determined
Lipoproteins don’t behave the same way in every body.
When metabolic health breaks down — insulin resistance, chronic inflammation, mitochondrial stress — several things happen at once:
LDL particles become smaller and more oxidizable
ApoB particle production rises
Lp(a) becomes more inflammatory
HDL loses protective function
Arteries become more vulnerable to damage
This is why inflammatory and metabolic markers matter so much.
Markers I personally track closely:
hs-CRP: 0.2
Homocysteine: 6
Fasting insulin: 2.3
That fasting insulin number matters more than most people realize. It reflects how hard the body needs to work to keep blood sugar stable — and by extension, how much metabolic stress arteries are exposed to day-to-day.
Low fasting insulin doesn’t mean zero risk — but it dramatically lowers the likelihood that lipoprotein particles will behave in a damaging way once they’re in circulation.
Think of insulin like traffic control. When it’s low and steady, particles move smoothly. When it’s chronically elevated, congestion builds — and that’s when accidents happen.
🧩 When LDL and ApoB Stay High Despite “Perfect” Markers
Here’s an important nuance that often gets overlooked.
Some people — myself included — are hyper-absorbers of dietary cholesterol.
In these cases:
LDL-C and ApoB can remain elevated
Even when triglycerides are low
Even when HDL is high
Even when inflammation and insulin resistance are minimal
My current snapshot:
LDL-C: 123
ApoB: 92
LDL pattern: A
Triglycerides: 48
HDL: 94
hs-CRP: 0.2
Homocysteine: 6
Fasting insulin: 2.3
For context: I know I’m a hyper-absorber because I’ve tracked my response to dietary cholesterol over time. When I increase foods like eggs, my LDL-C and ApoB rise predictably. I’ve kept my diet consistent, prioritized all the modifiable factors, and monitored trends longitudinally.
This is exactly why isolated numbers mislead.
The real question isn’t “Is LDL elevated?”
It’s “What’s the particle burden, what type are they, and what environment are they operating in?”
Advanced testing doesn’t give simple answers — it gives better ones.
🎛️ Which Markers You Can Improve — and Which You Can’t
Highly modifiable:
ApoB
Triglycerides
Inflammation (hs-CRP)
Homocysteine
Insulin sensitivity
HDL function
Context-dependent:
LDL-C (can rise or fall depending on absorption, production, and particle size)
Largely non-modifiable:
Lp(a)
Lp(a) is genetic. The strategy isn’t elimination — it’s de-risking around it:
Keep ApoB controlled
Keep inflammation low
Maintain strong metabolic health
Avoid stacking additional risk factors
Knowing which levers you can pull — and which you can’t — is the real upgrade.
🧠 The Real Takeaway
Heart disease isn’t a story of “bad cholesterol.”
It’s a story of:
Particle number
Genetics
Metabolic health
Inflammation
Insulin resistance
Oxidative stress
LDL-C tells one small part of that story.
ApoB, Lp(a), triglycerides, HDL context, and inflammatory markers tell far more — especially when interpreted together.
Advanced lipid testing doesn’t replace clinical judgment.
It sharpens it.
⚡ TL;DR
LDL-C measures cholesterol content, not particle risk
ApoB reflects total atherogenic particle number
Lp(a) is a powerful genetic risk factor most people never test
HDL and triglycerides provide metabolic context
Inflammation and insulin sensitivity determine how dangerous particles become
Risk lives in patterns, not single numbers
Until next week. Stay vital.
-Jordan Slotopolsky
📚 Sources
Sniderman AD et al., JAMA (2019)
Tsimikas S., New England Journal of Medicine (2017)
European Society of Cardiology Dyslipidemia Guidelines (2023)
American Heart Association Scientific Statement on ApoB (2022)
Ference BA et al., European Heart Journal (2017)
Cromwell WC & Otvos JD, Current Atherosclerosis Reports
Disclaimer:
The content provided in this newsletter is for informational and educational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this newsletter. The information provided does not constitute the practice of medicine or any other professional healthcare service.



